Immediately after diagnosis, MNT is initiated to reduce blood Phe concentrations, preventing the development of severe and often irreversible neurological, behavioral, and psychiatric symptoms.3



The healthcare community generally accepts that dietary management adds significant daily burden to patients and caregivers.9,10
*Online questionnaire was voluntarily completed and submitted by adults with PKU or parents/caregivers of children or adults unable to complete the survey themselves. The questionnaire was placed on the UK NSPKU website, Facebook, and Twitter accounts between November 9, 2017 and January 31, 2018.
In many regions, reimbursement of special manufactured low-protein foods and protein substitutes/medical foods remains an issue3
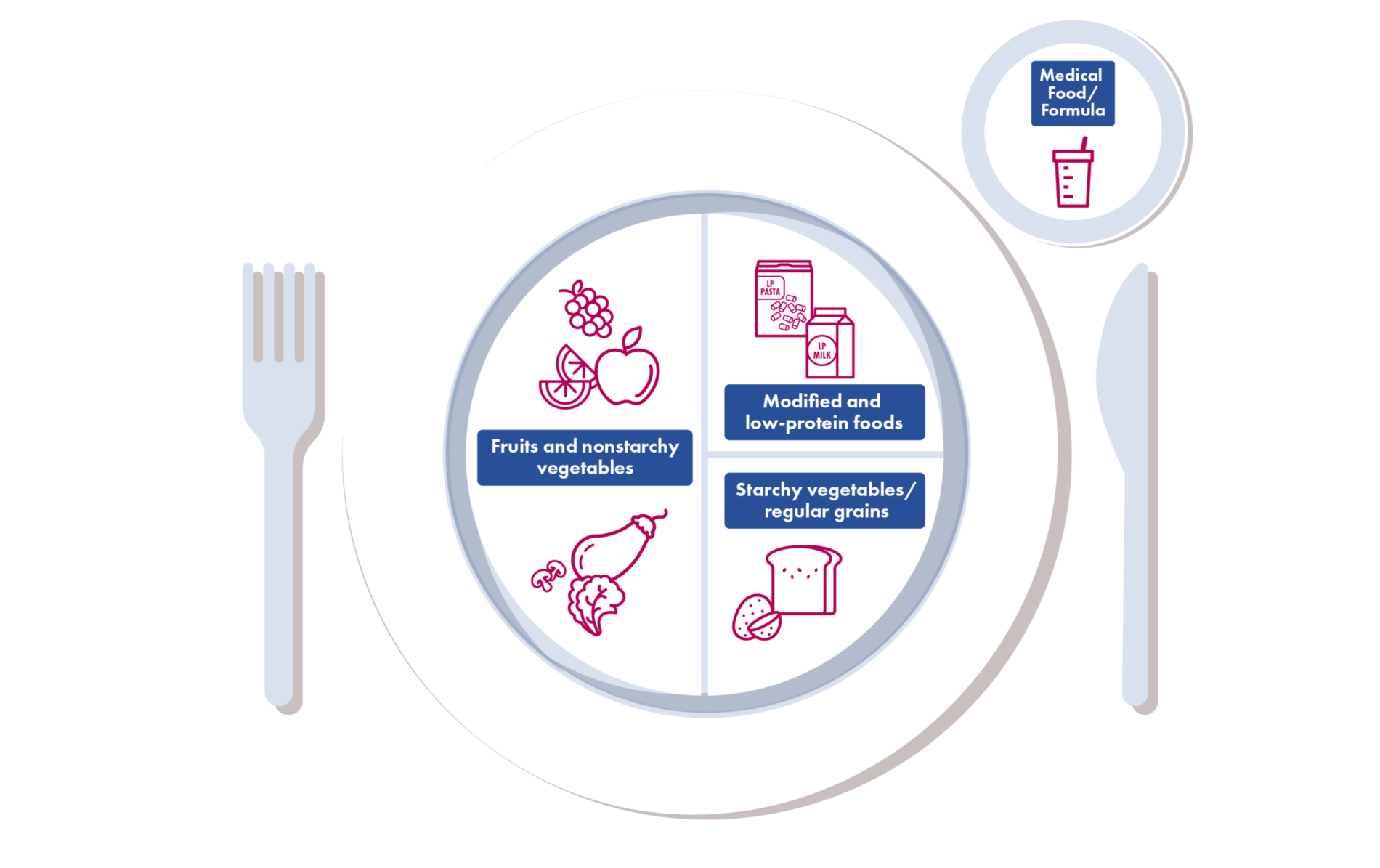
Even among patients who report dietary Phe restriction:
Many can experience elevated blood Phe levels, underscoring the inadequacy of this approach.

Eric: PKU Phe-restricted diet challenges
Hear how Eric overcame Phe-restricted diet challenges
and got back to a new kind of PKU care.
References: 1.Rocha JC, MacDonald A. Dietary intervention in the management of phenylketonuria: current perspectives. Pediatric Health Med Ther. 2016;7:155-163. 2. Vockley J, Andersson HC, Antshel KM, et al; American College of Medical Genetics and Genomics Therapeutic Committee. Phenylalanine hydroxylase deficiency: diagnosis and management guidelines. Genet Med. 2014;16(2):188-200. 3. Rocha JC, Ahring KK, Ausel H, et al. Expert consensus on the long-term effectiveness of medical nutrition therapy and its impact on the outcomes of adults with phenylketonuria. Nutrients. 2023;15(18):3940. 4. Lehman S. What to eat when you have PKU. Dietary recommendations for better management. Verywell Health. Updated July 12, 2023. Accessed December 22, 2023. https://www.verywellhealth.com/what-is-the-pku-diet-2507160. 5. van Wegberg AMJ, MacDonald A, Ahring K, et al. The complete European guidelines of phenylketonuria: diagnosis and treatment. Orphanet J Rare Dis. 2017;12(1):162. 6. MacLeod EL, Ney DM. Nutritional management of phenylketonuria. Ann Nestle (Engl) 2010;68:58-69. doi:10:1159/00312813. 7. US Department of Agriculture. Agricultural Research Service/Food Data Central/Food Search. 8. Enns GM, Koch R, Brumm V, Blakely E, Suter R, Jurecki E. Suboptimal outcomes in patients with PKU treated early with diet alone: revisiting the evidence. Mol Genet Metab. 2010;101(2-3):99-109. 9. Ford S, O’Driscoll M, MacDonald A. Living with phenylketonuria: lessons from the PKU community. Mol Genet Metab Rep. 2018;17:57-63. 10. van Spronsen FJ, van Wegberg AMJ, Ahring K, et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017;5(9):743-756. 11. Trefz FK, van Spronsen FJ, MacDonald A, et al. Management of adult patients with phenylketonuria survey results from 24 countries. Eur J Pediatr. 2015;174(1):119-127. 12. Levy H, Lamppu D, Anastosoaie V, et al. 5-year retrospective analysis of patients with phenylketonuria (PKU) and hyperphenylalaninemia treated at two specialized clinics. Mol Genet Metab. 2020;129(3):177-185.