
*P<0.05.
Abbreviations: ADD, attention deficit disorder; ADHD, attention deficit hyperactivity disorder.
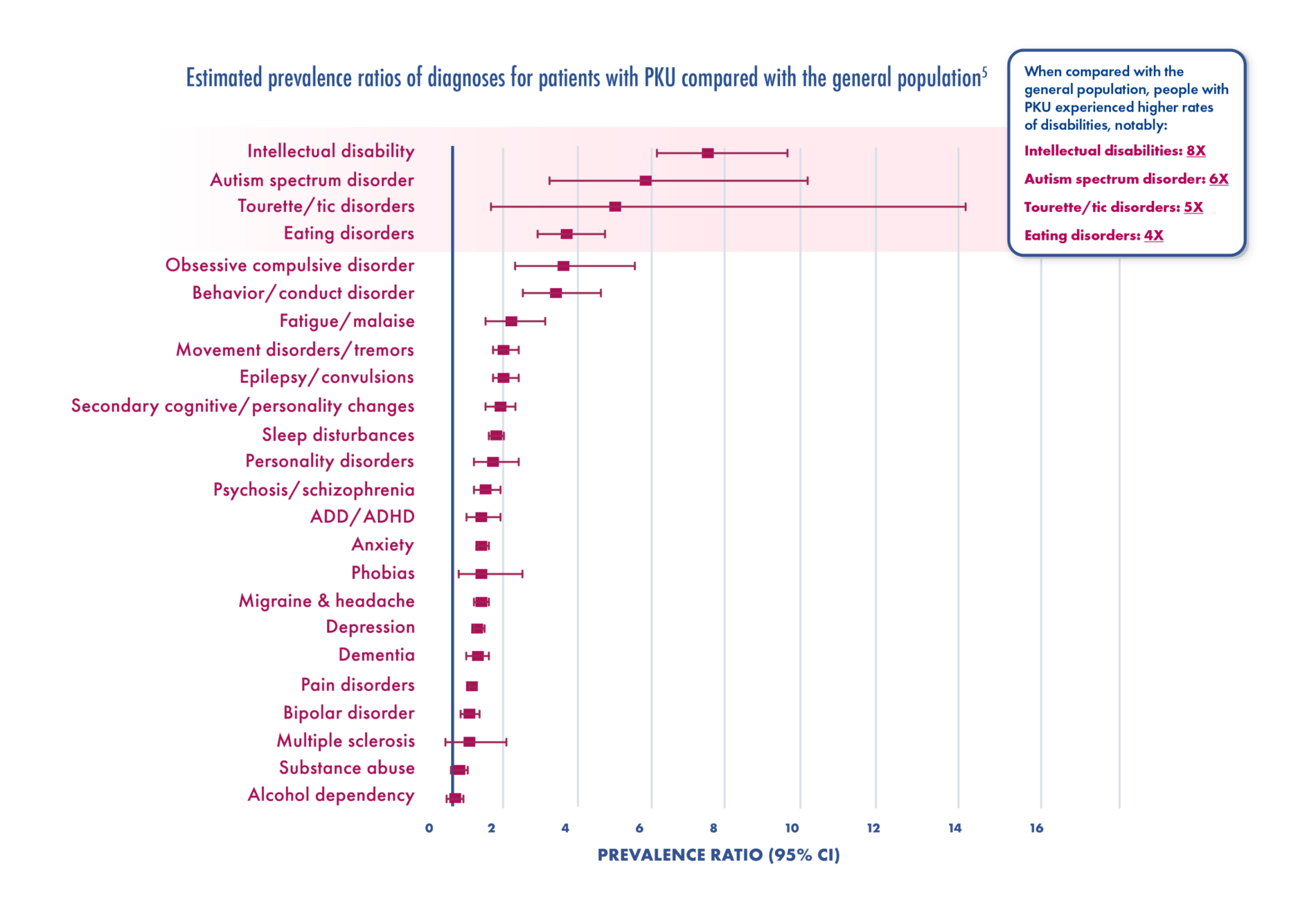
Adapted from Bilder et al. Mol Genet Metab. 2017.
Comprehension, ability to complete tasks, and school or work performance
Ability to hold information in mind that will be used to guide one’s actions; whether now or at a later point in time
Ability to sustain attention or persistence of effort with tasks
Self-regulation, such as control to avoid “off-limit” foods and refrain from outbursts or challenging behavior (critical for fulfilling responsibilities of adulthood)
Thinking out acts and purposes in advance; examples include meal planning, task planning, and thought organization
Even patients with blood Phe ≤500 μmol/L in childhood showed a higher frequency of psychiatric diagnoses, such as:


When you can cause irreversible brain damage to your child, it causes a lot of worry, stress, and even panic.11
Parent
I have blank moments where I can’t think or get my words out that I am trying to say. I experience anxiety and I get paranoid.11
Patient with PKU
I get “brain fog”, tend to become irritable and uneasy in social settings.11
Patient with PKU
Adults with PKU have an increased risk of several multisystemic comorbidities
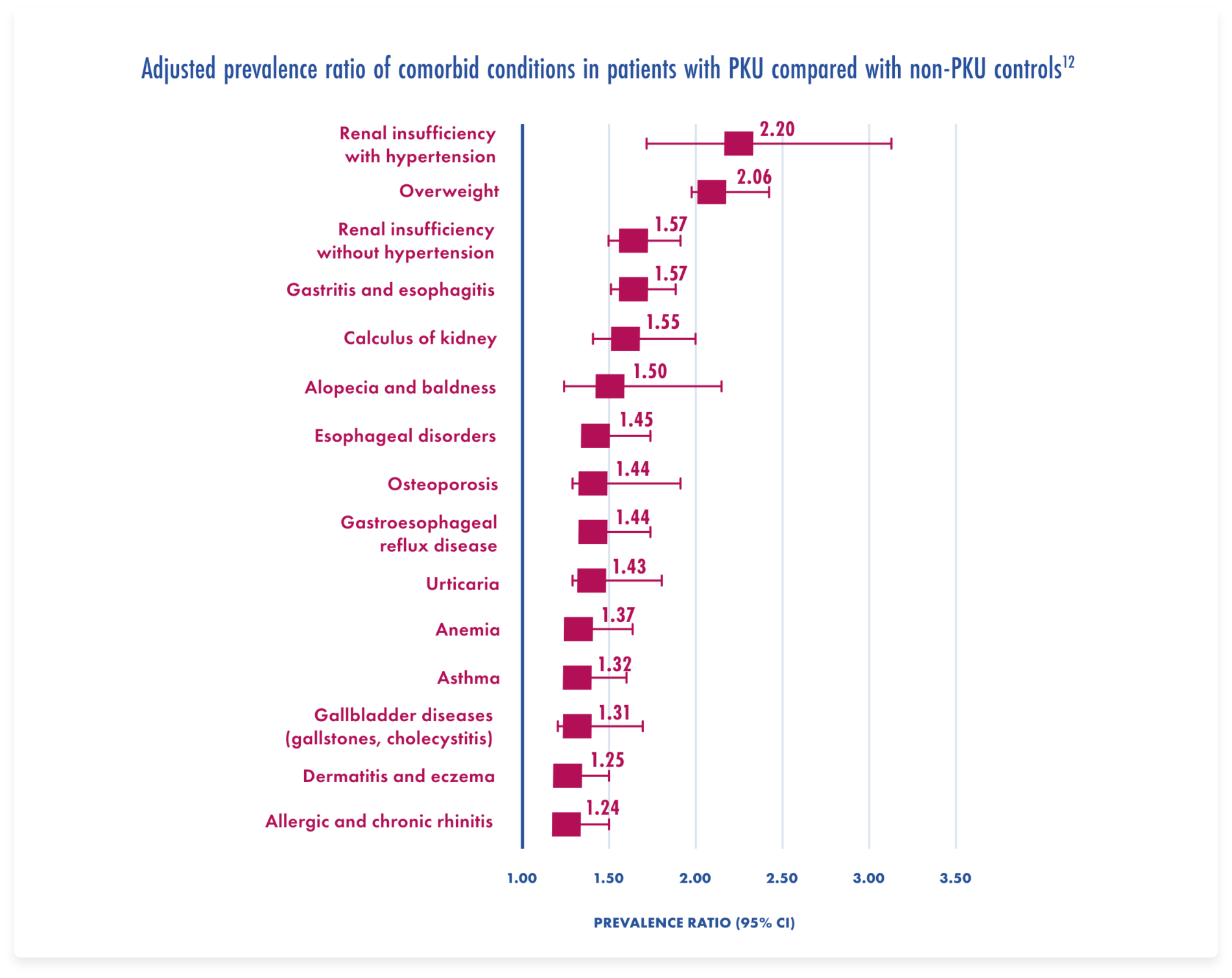
Adapted from Burton et al. Mol Genet Metab. 2018.
Connie: Learning to Focus on Herself
See how returning to clinic afer 50 years helped Connie achieve the best Phe levels of her life.
References: 1. Vockley J, Andersson HC, Antshel KM, et al. American College of Medical Genetics and Genomics Therapeutic Committee. Phenylalanine hydroxylase deficiency: diagnosis and management guidelines. Genet Med. 2014;16(2):188-200. 2. ten Hoedt AE, de Sonneville LMJ, Francois B, et al. High phenylalanine levels directly affect mood and sustained attention in adults with phenylketonuria: a randomised, double-blind, placebo-controlled, crossover trial. J Inherit Metab Dis. 2011;34(1):165-171. 3. Trefz KF, Muntau AC, Kohlscheen KM, et al. Clinical burden of illness in patients with phenylketonuria (PKU) and associated comorbidities―a retrospective study of German health insurance claims data. Orphanet J Rare Dis. 2019;14(1):181. doi:10.1186/s13023-019-1153-y. 4. Ashe K, Kelso W, Farrand S, et al. Psychiatric and cognitive aspects of phenylketonuria: the limitations of diet and promise of new treatments. Front Psychiatry. 2019;10:561. doi:10.3389/fpsyt.2019.00561. 5. Bilder DA, Kobori JA, Cohen-Pfeffer JL, Johnson EM, Jurecki ER, Grant ML. Neuropsychiatric comorbidities in adults with phenylketonuria: a retrospective cohort study. Mol Genet Metab. 2017;12(1):1-8. 6. van Wegberg AMJ, MacDonald A, Ahring K, et al. The complete European guidelines of phenylketonuria: diagnosis and treatment. Orphanet J Rare Dis. 2017;12(1):162. doi: 10.1186/s13023-017-0685-2. 7. Bone A, Kuehl A, Angelino A. A neuropsychiatric perspective of phenylketonuria I; overview of phenylketonuria and its neuropsychiatric sequelae. Psychosomatics. 2012;53(6):517–523. 8. Bilder DA, et al. Systematic review and meta-analysis of neuropsychiatric symptoms and executive functioning in adults with phenylketonuria. Dev Neuropsychol. 2016;41(4):245-260. 9. Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135-168. 10. Manti F, Nardecchia F, Chiarotti F, Carducci C, Leuzzi V. Psychiatric disorders in adolescent and young adult patients with phenylketonuria. Mol Genet Metab. 2016;117(1):12-18. 11. Ford S, O’Driscoll M, MacDonald A. Living with phenylketonuria: lessons from the PKU community. Mol Genet Metab Rep. 2018;17:57-63. 12. Burton BK, Jones KB, Cederbaum S, et al. Prevalence of comorbid conditions among adult patients diagnosed with phenylketonuria. Mol Genet Metab. 2018;125(3):228-234. 13. Brown CS, Lichter-Konecki U. Phenylketonuria (PKU): a problem solved? Mol Genet Metab Rep. 2016;6:8-12. 14. Jurecki ER, Cederbaum S, Kopesky J, et al. Adherence to clinic recommendations among patients with phenylketonuria in the United States. Mol Genet Metab. 2017;120(3):190-197. 15. van Spronsen FJ, van Wegberg AMJ, Ahring K, et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017;5(9):743-756.